It is one of the vaginitis more prevalent in the life of the woman, it is caused by a fungus which colonizes the digestive (up to 80% of the population) and genital tracts (20%) of normal adults, so it is not considered a sexually transmitted infection.
There are people with asymptomatic vaginal infections and others suffering from classic symptoms of the infection. Treatment is usually very simple and includes treatment of the couple as is considered necessary to limit the asymptomatic infection in the sexual partner (male or female) to prevent recurrences; preventive measures are very important, read this article: care of the Vulva
What is the vaginal yeast infection?
Candidiasis is an infection caused by candida albicans (85%), C. glabrata (5-10%), and C. tropicalis (5%), agents that have as a reservoir to the digestive tract, skin, and nails. In sensitive patients it causes a symptomatic colonization of the region vaginal vulvo manifested by vaginal discharge grumoso and irritant.
Changes in immunity, lifestyle and hormonal State favour the emergence of symptomatic infection in women: pregnancy, use of oral contraceptives, antibiotics, changes in diet and body weight, diabetes, use of towels daily and sex orogenital. Due to lack of estrogen, once rare post-menopausal women suffering vaginal candidiasis
What are the symptoms of thrush?
Some women are asymptomatic carriers of the fungus (20-80%), and other manifest symptoms of genital itching in the presence of a vaginal grumoso, white, no particular smell that causes burning in the vulvar region. Due to the proximity of the urethra infection Candida it can simulate a low urinary tract infection or cystitis. In immunosuppressed patients may be urinary tract infection Candida, cystitis, or generalized infections involving life.
The symptoms of genital candidiasis becomes more intense or appears before menses, after the bath or while lying in her bed mildly wrapped.
How is it diagnosed?
Clinical characteristics of infection can make the diagnosis in the majority of cases without any particular evidence more than the traditional gynecological exam: the vulva looks red and irritated, the vaginal walls show signs of irritation with the presence of an adherent grumoso vaginal walls. If there are questions you can study with a microscope or a sample for culture
What treatment is needed?
There are various oral and topical antifungal preparations. In general, the treatment takes 1 to 7 days. More than 90% of women are cured with simple treatments of short duration; It is very important to treat the sexual partner of the patient to ensure cure of the infection. In approximately 48 hours after starting treatment symptoms have practically disappeared. In difficult infections are designed special treatment schemes; the C glabrata is resistant to traditional schemes.
Recurrent candidiasis: > 4 episodes per year
It should be treated with vaginal suppository for 10-14 days and fluconazole 150 mg VO, weekly for 6 months. A 40-50% relapse rate is expected by the end of this therapy. Risk factors should be monitored.
What I have and I do not do
- Yearly visit to your gynecologist, reports on the recent use of antibiotics and the presence of other risk factors.
- Use cotton underwear and avoid tight and synthetic garments.
- Controlling your weight and your chronic diseases, especially diabetes.
- You do not practise Vaginal Douches (banned in modern Gynecology).
- Not you asees from behind to ahead after evacuating.
- Do not use sanitary towels daily, maintaining constant genital moisture and promote the persistence of the fungus causing chronic irritation and vulvar aging aspacto.
- Do not use synthetic fabrics underwear or tight clothing.
- You do not believe: the diagnosis than your think it is not correct, you will use a medicine that you will not cure, you will lose time and money.
- Perhaps it is good idea to leave some vulvar pubic hair to encourage genital moisture evaporation and avoid direct contact with the panty.
- Be sure to implement all the recommendations on the care of the vulva.
The causal agent
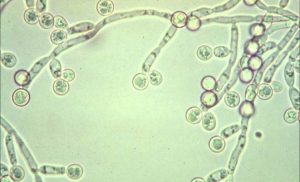
Candida albicans microscope fresh.
-

- Candidiasis genital con irritación vulvar severa asociada al uso de toallas sanitarias diarias.
-

- Colonias en infección severa
-

- Colonias en infección leve
Genital candidiasis, the fungus colonies lining the surface of the cervix, and part of the vaginal walls in severe cases.
Prevention
- Avoid prolonged and excessive moisture in the area.
- Avoid the chronic use of towels daily protection, look at its effects:
-

- Evite el uso crónico de toallas de protección diaria, mire sus efectos: vulvovaginitis por candidiasis severa
-

- Después. Suspendió el uso de toallas diarias y recibió tratamiento.
-
- Use baby powder on skin folds to avoid maceration if you have overweight or obesity, control your weight
- Avoid the use of synthetic fabrics underwear, use cotton
- Let the cigarette
- Avoid broad-spectrum antibiotics
- Avoid the use of steroids
- If you visit swimming pools or beaches do not remain wet swimsuits for long periods of time
- Sex in the shower or in a body of water (pool, sea) generates a strong vaginal wash that removes the normal vaginal flora making it prone to infections by fungi and bacterial vaginosis